In insurance, 70% of inbound claims calls don’t need a human, yet agents stay overloaded. AI claims automation tackles routine queries and status checks upfront, freeing teams for complex work and better claimant experiences. As the industry shifts toward smarter, leaner operations, the question becomes: how far can this automation go for your claims org?
Shift FAQs to AI for smoother CX.
Why AI Claims Automation Matters When 70% Of Calls Don’t Need A Human
Instead of diving headlong into AI claims automation, here’s a quick definition to guide your search: AI claims automation is the use of AI-driven systems to handle routine claims interactions, Such as status checks and simple queries, before they reach agents, reducing call volume and improving operational efficiency across insurance teams.
Most insurance leaders don’t realize a quiet truth hiding in their contact center metrics: the majority of incoming calls never needed a human in the first place. Simple questions, predictable patterns, and status updates flood already stretched teams. This is exactly where AI claims automation steps in, not as a replacement for agents, but as a relief valve that preserves human effort for truly human problems.
For years, claims teams have been expected to perform at high empathy and high accuracy under mounting pressure. Yet 70% of claimants call only because self-service feels unreliable or incomplete. With AI claims automation, carriers can finally redirect that volume before an agent even hears the phone ring.
Handle Routine Insurance Queries
Most claims calls begin with a predictable rhythm: “What’s the status of my claim?” “What documents do I still need?” “When will someone get back to me?” These are precisely the low-value but high-frequency moments that agents handle repeatedly. Automating this layer with AI claims automation changes the flow entirely, especially when customers expect instant resolution.
Because handling routine insurance queries is a critical operational lever, leaders can’t ignore how much capacity it drains. When AI claims automation picks up these queries first, customers get fast clarity, and agents get their time back.
By ensuring systems can handle routine insurance queries before humans get involved, carriers reduce friction on both sides of the call. Add AI claims automation into that first-touch layer, and these queries feel less like burdens and more like painless CX opportunities.
Insurance Claims Status Automation
There’s no bigger magnet for unnecessary inbound traffic than claims status checks. Customers feel stuck unless they call, even though status information already exists behind the scenes. This is why insurance claims status automation pairs perfectly with AI claims automation: it surfaces that buried data in real time, eliminating the need for manual intervention.
Customers simply want transparency. Insurance claims status automation gives them exactly that, and when powered through AI claims automation, the experience becomes proactive, accessible, and instant.
With insurance claims status automation consistently delivering answers before a human is needed, call volume naturally drops. And when this experience is orchestrated through AI claims automation, the claims journey feels modern, responsive, and trust-building.
Once routine queries and status checks are automated at the front door, the next question becomes: What else can AI remove from your call queues before a human gets involved? That’s where the flow of automation becomes even more powerful.
Offload status checks to AI in minutes.
How AI Claims Automation Quietly Removes Low-Value Calls
When implemented well, AI claims automation becomes the invisible workforce handling the work that no agent should be spending time on. It authenticates callers, identifies intent, answers questions, and escalates only when complexity or emotion requires a human touch. The result is a calmer claims floor and a better claimant experience.

Intelligent Call Routing For Insurance
Traditional IVRs send callers down rigid menus, leading to frustration and misroutes. Intelligent call routing for insurance works differently: it listens first, then decides. When paired with AI claims automation, intent detection becomes dynamic, context-aware, and significantly more accurate.
As carriers upgrade workflows, intelligent call routing for insurance becomes a backbone capability that supports lower transfers, cleaner workflows, and higher CSAT.
By introducing intelligent call routing for insurance, teams ensure calls reach the right destination instantly. Combined with AI claims automation, routing becomes smarter, faster, and far more aligned with real customer needs.
Claims Operations Efficiency
Every insurer is under pressure to do more with less, fewer resources, tighter timelines, and higher customer expectations. Claims operations efficiency becomes nearly impossible when agents are drowning in repetitive calls. With AI claims automation, carriers can finally reclaim control over time, workflows, and utilization.
As volume stabilizes, claims operations efficiency improves naturally, not because teams work harder, but because the system works smarter.
The compounding effect is real; higher claims operations efficiency, lower handle times, and happier agents all emerge from consistent use of AI claims automation at the earliest stages of a claim.
Automation removes the noise, but the real magic happens when teams finally have space to do meaningful work. Let’s explore what that shift looks like.
Upgrade first-touch claims calls.
This blog is just the start.
Unlock the power of Convin’s AI with a live demo.

What Happens To Your Team When AI Claims Automation Handle Calls
When AI claims automation absorbs repetitive work, something surprising happens: agents get to be specialists again. Instead of cycling through hundreds of basic calls, they finally focus on complex investigations, fraud checks, negotiation, and claimant guidance, the tasks that require experience and empathy.
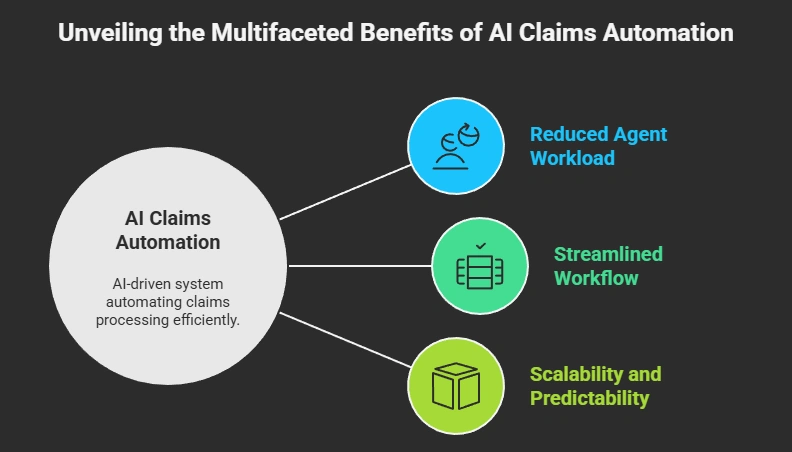
Agent Workload In Claims
High agent workload in claims is a direct contributor to burnout, attrition, and quality issues. Most teams aren’t overwhelmed because claims are harder; they’re overwhelmed because simple calls never stop coming. With AI claims automation, the load eases immediately, redistributing energy toward specialized work.
As agent workload in claims decreases, coaching becomes more effective, and performance metrics stabilize.
Reducing agent workload in claims isn’t just about efficiency; it’s about protecting the people who carry the claims experience. AI claims automation gives them breathing room to do their best work.
Insurance Contact Center Automation
Claims leaders increasingly rely on insurance contact center automation to modernize their operations without increasing headcount. When routine tasks shift to AI, teams become more strategic and less reactive. AI claims automation becomes the operational backbone that keeps work flowing smoothly.
Insurance contact center automation doesn’t replace agents; it prevents overload.
By integrating insurance contact center automation with conversational AI flows, carriers create predictable, scalable service. And at the center of that system sits AI claims automation, ensuring only meaningful calls reach human experts.
Now that the human impact is clear, it’s useful to understand how Convin fits into this journey.
Automate your claim FAQs instantly.
Where Convin Fits In The AI Claims Automation Journey
Convin enters the story quietly, more as an enabler than a disruptor. Its automated virtual AI agents (AI phone calls) carry out routine calls, status updates, reminders, and FAQs with precision. Within the broader world of AI claims automation, Convin simply helps insurers make the jump faster, without ripping out existing systems.
Human Agents vs. Automated Virtual AI Agents

1. Routine Calls
How human agents handle it:
A claimant calls asking a predictable question. The agent pulls up the CRM, verifies identity, navigates claim notes, gives a short answer, and moves to the next call. By mid-shift, they’ve handled the same query 40+ times: fatigue grows, quality slips, and queues build.
How automated virtual AI agents handle it:
The AI answers instantly, authenticates the caller, retrieves claim details, and responds in seconds. No hold times, no repetition fatigue, no queue buildup, just scalable handling of routine calls without draining human attention.
2. Status Updates
How human agents handle it:
The caller asks, “Where is my claim right now?” The agent checks multiple systems, decodes back-end notes, and explains the stage in plain language. It’s straightforward but time-consuming, and every minute adds to overall handle time.
How automated virtual AI agents handle it:
The AI accesses real-time status data, translates system language into simple updates, and communicates the next expected step automatically. It can give status updates 24/7 and instantly, preventing next-day call spikes and reducing unnecessary agent load.
3. Reminders
How human agents handle it:
Agents send reminders manually or during follow-up calls, document submissions, missing information, and scheduled adjuster visits. Work often depends on task lists, memory, and available bandwidth, leaving room for delays.
How automated virtual AI agents handle it:
The AI triggers reminders automatically based on workflow rules, calling customers to nudge document submissions, confirm appointments, or clarify pending steps. Every reminder goes out on time, with consistent messaging and no manual effort.
4. FAQs
How human agents handle it:
Agents repeat the same explanations all day: coverage basics, turnaround expectations, deductible clarifications, and what counts as supporting evidence. Each answer is simple, but collectively drains hours from the team.
How automated virtual AI agents handle it:
The AI answers FAQs instantly with consistent accuracy, using approved knowledge bases and insurer-specific language. It adapts intent, asks follow-up questions, and provides clear responses without the variability or fatigue common in human-led interactions.
AI For Claims Customer Service
Modern claimants expect immediacy, accuracy, and empathy. AI for claims customer service sits at the intersection of all three. Convin’s approach allows basic interactions to stay automated while nuanced or emotional cases reach real agents. Pair this with AI claims automation, and you get a seamless, always-available service layer.
AI for claims customer service elevates the moments where humans are most needed.
With AI for claims customer service powering the claimant experience and AI claims automation streamlining operations, insurers build a claims journey that feels modern, responsive, and deeply human, ironically because much of the noise is handled by machines.
Once automation, human expertise, and intelligent routing align, the claims function begins to operate at its highest potential. Now let’s bring it home.
Schedule a Convin demo now!
AI Claims Automation As The Fastest Path To A Healthier Claims Org
Claims organizations can’t scale if humans remain the frontline for low-value interactions. But with AI claims automation, the path forward becomes clearer: automate the predictable, elevate the meaningful, and rebuild the experience around speed and accuracy.
When 70% of calls never reach agents, teams finally thrive.
In the end, AI claims automation is not about cutting humans out; it’s about giving them better work, better focus, and better outcomes. If you’re exploring this shift, consider taking a small diagnostic to see what’s possible. Change starts with one automated claim call.
FAQs
1. How does AI claim automation reduce repeated caller inquiries?
AI claims automation provides real-time answers to status checks and FAQs, preventing customers from calling multiple times for the same information.
2. Can AI claims automation improve claimant transparency?
Yes. It delivers instant updates and clarifies next steps, reducing uncertainty and frustration that often trigger unnecessary calls.
3. Do AI claims automation help with after-hours call volume?
AI claims automation operates 24/7, resolving routine queries when agents are offline and preventing next-day call spikes.
4. How fast can insurers deploy AI claims automation?
Most teams can deploy it in phases, starting with routine queries and expanding to more workflows as accuracy improves.
5. What data does AI claims automation need to function effectively?
It typically requires access to claims status, customer authentication data, and policy details to respond accurately and reduce agent dependency.







.avif)