Insurance claims automation is rapidly transforming the insurance industry by streamlining claim settlements and improving accuracy. Leveraging robotic process automation in insurance claims processes accelerates every step from FNOL to fraud detection and payout. This reduces costs, enhances compliance, and boosts policyholder satisfaction. Leading insurers that utilize Convin’s automation solutions experience faster claims handling, improved operational efficiency, and enhanced customer trust.
Insurance claims automation refers to the use of technology to streamline and expedite the processing of claims. It reduces manual tasks, improves accuracy, and accelerates settlements, resulting in faster payouts and enhanced customer satisfaction. This approach helps insurers lower costs, detect fraud early, and ensure compliance throughout the claims lifecycle.
Let’s explore how insurance claims automation with RPA drives measurable benefits, shaping the future of claims management and competitive advantage.
Integrate Convin for seamless claims data accuracy and speed!
Why Insurance Claims Automation Matters Today
The insurance industry stands at a pivotal moment of digital transformation. Rising claim volumes, higher customer expectations, and tighter economic margins demand stronger operational agility. Manual processes are proving inadequate, creating inefficiencies and delays.
- Insurance claims automation directly addresses these challenges by removing operational bottlenecks.
- It digitizes repetitive workflows, allowing insurers to achieve faster, more accurate, and cost-effective claims settlements.
- This directly impacts customer satisfaction and policyholder retention.
Executives confirm automation is reshaping the competitive dynamics of the industry. Insurance carriers relying on robotic process automation in their insurance claims operations deliver superior customer experiences. They achieve higher profitability through reduced costs and minimized compliance risks.
RPA In Claims Handling
RPA in claims handling replicates human actions, executing structured claim processes swiftly and consistently. It automates tasks such as validations, acknowledgments, and settlement calculations, eliminating the need for human intervention. This significantly reduces human error and processing delays.
- Insurance leaders deploying RPA in claims handling report that routine processes scale effortlessly during flood or catastrophe events.
- The solutions adjust claims load without hiring temporary staff.
- Customers experience consistent resolution times even during claim surges.
RPA in claims handling also creates transparency by updating claimants digitally. Claimants can track progress without waiting for agents. This transparency fosters loyalty and significantly decreases inbound support call volumes.
RPA For Claims Data Entry
RPA for claims data entry solves one of the most operationally expensive functions for insurers. Processing documents manually from customer policies, medical records, and accident files typically consumes hours of staff effort. Automation reduces this to minutes.
- RPA for claims data entry extracts information using OCR and pre-trained rules.
- This structured data is then validated and seamlessly entered into core systems.
- It eliminates errors that cause settlement delays and unnecessary customer dissatisfaction.
Executives highlight measurable ROI through automation-enriched accuracy. Fewer reworks and disputed claims save insurers millions annually. By automating entry, staff can focus on fraud detection and relationship-building instead of repetitive typing tasks.
Insurance claims automation begins with efficient intake but scales across the entire claims journey. We now explore how robotic process automation (RPA) is integrated across multiple touchpoints to accelerate the delivery of insurance claims.
Transform FNOL with Convin’s Real-Time Agent Assist insights!
How Insurance Claims Automation Works With RPA
Insurance claims automation, powered by RPA, delivers measurable efficiency gains by seamlessly connecting every stage of the claims process. RPA performs tasks previously reliant on manual efforts, reducing cycle times from intake to payout. This results in faster, compliant, customer-first outcomes.
RPA For FNOL
RPA for FNOL (First Notice of Loss) revolutionizes the critical first notice of loss stage. Unlike traditional models, where agents manually transcribe details, automation immediately captures claim data from customer calls, emails, and portals. It directly routes structured details into claims systems.
- This removes duplication errors caused by manual handling.
- Policyholders experience faster claim acknowledgment and immediate confirmation of validation.
- Automated intake ensures that critical information is not lost during event escalation periods.
Insurers note that implementing RPA for FNOL significantly improves customer trust. Prompt acknowledgment demonstrates insurer commitment. It also empowers downstream automation, such as fraud detection and policy scans, drastically reducing settlement cycles.

RPA Claims Fraud Detection
Fraud remains one of the largest burdens on the industry, costing insurers billions in false claim settlements. RPA claims fraud detection identifies suspect submissions by automatically applying algorithms and analytics to claim history, behavior, and data anomalies.
- Unlike manual checks, RPA claims fraud detection operates round-the-clock with scalable monitoring of incoming claims.
- It cross-references multiple databases to spot duplicate claims, suspicious injuries, or unusual claim activity patterns without silos.
Executives recognize immediate cost reduction with automation-led detection.
- Resources previously wasted on payouts for fraudulent claims are reallocated to genuine payouts.
- This approach improves industry credibility while uplifting policyholder trust in claim fairness.
While intake and fraud detection are critical, broader lifecycle improvements are equally important. The next stage highlights the specific advantages that insurance carriers unlock through robotic process automation in insurance claims solutions.
Drive faster claim settlements using Convin’s end-to-end automation.
This blog is just the start.
Unlock the power of Convin’s AI with a live demo.

Benefits of Robotic Process Automation in Insurance Claims
Insurance claims automation ensures benefits that ripple across the claims lifecycle. From intake to settlement, automation enhances accuracy, reduces costs, and strengthens adherence to compliance. The result is measurable operational and financial ROI.
Improved Compliance Through Policy Administration Robotic Process Automation
Policy administration robotic process automation ensures claims remain compliant with regulatory standards throughout the lifecycle. Automated audit trails document every decision, improving accountability in highly regulated insurance landscapes.
- Insurers benefit by reducing compliance penalties and audit stress.
- Systems validate claim details automatically against policies, reducing human oversight errors.
- Automation ensures standardization of documentation and reporting.
Executives confirm that adopting policy administration robotic process automation improves governance confidence. Compliance adherence becomes proactive instead of corrective, positioning insurers as trustworthy and regulation-aligned entities in competitive markets.
Cost Reduction With RPA Insurance
RPA insurance directly cuts costs in claims processing. By automating functions such as data entry, fraud detection, and lifecycle management, insurers can reduce process redundancy and staffing expenses. The operational savings become massive in high-volume claims markets.
- These cost reductions extend beyond employee savings.
- Lower infrastructure requirements, reduced reworks, and faster cycle times improve profitability.
- Executives confirm RPA insurance allows improved budgeting flexibility for innovation initiatives.
Insurers utilizing RPA insurance significantly strengthen their financial stability. Leaner operations drive shareholder confidence while freeing investment capital. Cost efficiency, coupled with improved service, sustains long-term growth momentum.
Enhanced Customer Experience With Insurance Claims Automation
The speed and transparency of settlement claims directly impact customer satisfaction. Insurance claims automation streamlines end-to-end interactions. Claimants experience reduced inquiry delays, improved updates, and faster visibility of payouts.
- Transparency created by tools like RPA claims management software strengthens customer trust.
- Real-time communication from claim initiation to closure ensures fewer disputes and smoother engagements. Policyholders develop trust in automated ecosystems.
Executives note improved Net Promoter Scores, higher renewal rates, and enhanced capabilities for relationship building. By prioritizing automation, insurers can deliver customer-first service models that are critical for competitive differentiation.
Claims Lifecycle Automation RPA
Claims lifecycle automation RPA enables complete end-to-end automation of insurance claim workflows. Each stage, from notification and validation to fraud stamping and settlement approval, runs seamlessly. This creates consistent customer journeys from report to payout.
- Insurers adopting claims lifecycle automation RPA drastically reduce cycle time, moving from 14 days to under 5.
- Policyholder transparency in claims resolution continues to grow stronger, driving higher satisfaction scores across multiple survey metrics.
This operational harmony strengthens market resilience for insurers. Delays become exceptions, not the standard. By combining workforce and automation, insurers ensure continuous availability without incremental infrastructure escalations.
RPA Claims Management Software
RPA claims management software serves as a centralized platform integrating automation with claims workflows. It manages adjudication, communications, and cross-system data integrations. The software scales rapidly without requiring infrastructure overhauls, which is particularly important during seasonal claim surges.
- Insurers highlight RPA claims management software improves compliance readiness. Audit logs are generated automatically, enabling regulators to validate claims processing swiftly.
- This reduces the risks of penalties and strengthens governance standards.
Executives demonstrate that RPA claims management software enhances visibility of claims for all stakeholders. Customers track cases digitally. Managers access detailed analytics. Agents benefit from error-free adjudications supported by data reliability.
Organizations benefit from technology, but vendor-enriched value accelerates outcomes. Insurers are now exploring how Convin amplifies results from insurance claims automation using RPA.
Achieve measurable ROI via Convin’s claims lifecycle automation.
Convin’s Role In Accelerating Insurance Claims Automation
Convin delivers critical support to insurers seeking to accelerate their insurance claims automation. It integrates with existing frameworks to supercharge outcomes while maintaining compliance standards of BFSI environments. Executives consistently realize measurable ROI improvements post-implementation.
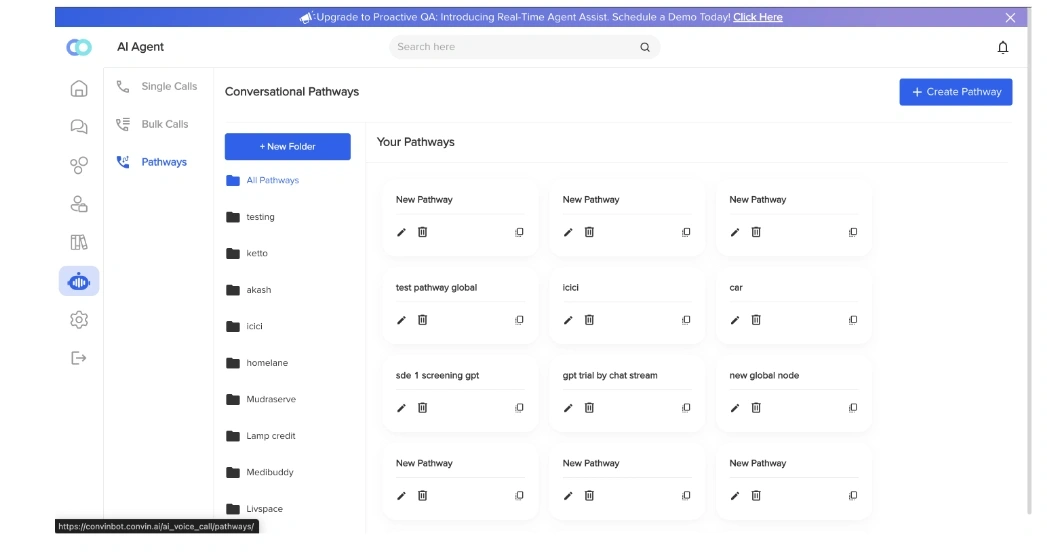
Real-Time Product Capabilities:
- Real-Time Agent Assist: Convin’s Real-Time Agent Assist equips insurance agents with on-screen, contextual prompts during live customer interactions.
It analyzes conversations in real-time, suggesting next best actions tailored to claims inquiries, FNOL processing, or settlement discussions.
By reducing guesswork and repetitive follow-ups, agents resolve queries more quickly, resulting in higher first-call resolution rates.
- Conversation Intelligence: With Conversation Intelligence, Convin captures, transcribes, and analyzes every customer conversation across contact centers and digital channels.
It uncovers actionable insights about claim delays, customer frustrations, and recurring issues within claims lifecycle automation RPA workflows.
This intelligence empowers executives with strategic data, while helping agents continually improve service quality and adherence to compliance.
- Automated Quality Assurance: Automated Quality Assurance continuously monitors 100% of customer-agent interactions without manual sampling delays.
It detects miscommunication, regulatory breaches, or inaccurate claim processing steps within seconds.
This ensures policy administration robotic process automation workflows remain error-free, compliant, and trustworthy.
Supervisors gain comprehensive visibility to coach staff better and enforce consistency across every claim engagement.
Core Use Cases Delivered:
- High-Volume Call Handling: Convin’s automation handles surges in claim-related calls seamlessly.
Real-time agent assistance and conversation intelligence ensure that every caller receives quick, accurate responses during peak claim periods, such as natural disasters.
This minimizes wait times and prevents service breakdowns, improving overall policyholder satisfaction.
- Payment Reminders Automation: Automated payment reminders notify policyholders promptly about premium dues or claim-related payments.
This reduces missed payments and late fees while improving insurer cash flow.
The system utilizes conversational AI to personalize reminders, thereby increasing engagement success rates without requiring manual intervention.
- Payment Collection Automation: Convin’s platform streamlines payment collection through secure, automated channels.
It supports digital payments and real-time reconciliation with insurer systems, reducing human error and improving billing accuracy.
This reduces operational costs and accelerates premium collections, enabling better fund management.
- Compliance Monitoring: Automated quality assurance and conversation analytics ensure that every customer communication remains within regulatory guidelines.
This is crucial for claims processes that are subject to strict insurance compliance regulations.
Real-time alerts enable quicker resolution of potential breaches, protecting the insurer's reputation and reducing audit risks.
Executives deploying Convin in robotic process automation insurance claims reports improved efficiency and lower operational costs. Increased policyholder transparency strengthens retention, while compliance monitoring significantly reduces legal and audit risks.
Beyond product specifics, industry insights confirm measurable success in adoption. RPA insurance solutions deliver wide-ranging efficiency backed by statistics and case adoption success.
Reduce claim cycle times using Convin’s Conversation Intelligence.
RPA In Claims Handling: Stats And Use Cases
Global insurers have already confirmed ROI numbers, validating the use of insurance claims automation powered by RPA. Industry statistics demonstrate a measurable transformation, convincing even the most skeptical leaders about the scalability opportunities.
Data-Backed Adoption:
- 65% of insurers automated FNOL processes and experienced a 40% reduction in errors.
- RPA in claims handling improved settlement times by 60%, cutting customer churn risks.
- RPA claims fraud detection reduced fraudulent payouts by 30%.
- Claims lifecycle automation RPA reduced resolver headcount needs by 25% during peak surges.
- RPA insurance lowered compliance audit penalties by nearly 20%.
Real Success With RPA Insurance
Executives report that RPA claims management software assisted in mitigating peak season event surges without requiring additional hiring. Claims surges caused by natural disasters were processed with universal accuracy and superior customer transparency.
RPA insurance ensures claims supervisors manage workloads optimally. Claims lifecycle automation RPA demonstrates that settlement costs recover more quickly than those of competitors without automation. Policyholders experience supportive journeys, translating into renewals and referrals that strengthen market visibility.
Having proven efficiency with data-backed insights, it’s essential to examine the long-term outlook automation provides. This future relevance ties directly to insurance resilience and customer-first operational models.
The Future Of Insurance Claims Automation
Insurance claims automation, anchored by robotic process automation, has become a business mandate. No longer optional, it defines survival in competitive environments. Customers demand speed, precision, and transparency that manual methods cannot offer.
RPA for FNOL, RPA claims fraud detection, and RPA claims management software modernize every insurer service point. Convin’s conversation-driven automation complements this digital shift, empowering proactive agent support and compliance assurance. Together, technologies ensure efficient leadership.
Executives acknowledge that the future belongs to insurers aligning operational execution with automation-enriched customer management. Claims lifecycle automation RPA delivers scalability. Policy administration robotic process automation ensures regulatory strength. Together, they secure profitable insurance ecosystems.
Book your Convin demo now!
FAQs
- What are the compliance considerations when deploying conversational AI in regulated insurance markets?
Compliance considerations include ensuring data privacy and protection in accordance with regulations such as GDPR and HIPAA. Conversational AI must maintain transparent audit trails, secure consent for data use, and adhere to industry-specific guidelines, such as those established by FINRA or state insurance laws. Automated quality assurance tools help monitor conversations to prevent regulatory breaches and maintain compliance.
- How does edge computing enhance real-time risk assessment for connected vehicles?
Edge computing processes data locally on the vehicle or nearby devices, reducing latency. This enables real-time risk assessment by instantly analyzing driving behavior, environmental conditions, and vehicle performance. Faster decision-making enhances accident prevention, dynamic pricing, and the development of personalized insurance policies for connected vehicles.
- What KPIs should insurers track to measure the ROI of digital claims transformation projects?
Key KPIs include reducing claims processing time, increasing the first-time claim resolution rate, achieving operational cost savings, enhancing customer satisfaction scores, and improving the accuracy of fraud detection. Tracking these metrics enables insurers to quantify efficiency gains, cost benefits, and enhanced customer experiences resulting from digital claims automation.
- How can blockchain improve transparency in multi-carrier reinsurance agreements?
Blockchain creates an immutable, shared ledger that is accessible to all parties involved in reinsurance agreements. It increases transparency by securely recording policy details, claims history, and transactions in real-time. This reduces disputes, speeds up settlements, and enhances trust among multiple insurers and reinsurers.
- What cybersecurity best practices protect sensitive policyholder data in cloud-based insurance platforms?
Best practices include encrypting data at rest and in transit, implementing multi-factor authentication, conducting regular security audits, and adhering to industry standards such as ISO 27001. Insurance platforms should implement role-based access controls and continuous monitoring to detect and prevent unauthorized access to or breaches of sensitive data.


.webp)


%20BLOG10%20examples%20of%20artificial%20intelligence%20in%202024.webp)




.avif)