Fraud in insurance isn’t just a nuisance. It’s a serious operational threat that eats into profit margins, slows down claims processing, and damages customer trust.
In the U.S. alone, insurance fraud causes estimated losses of $308.6 billion every year, which adds nearly $900 to each policyholder’s premiums. Roughly 20% of claims are believed to contain some form of fraud.
Legacy fraud detection tools like rule-based filters and manual audits are struggling to keep up. Fraudsters are using more sophisticated tactics: staged auto accidents, inflated health claims, organized rings, and even AI-generated fake documents.
Meanwhile, your teams are overwhelmed with false positives, investigations take too long, and legitimate claims are delayed. The result is higher costs and poor customer experience.
Convin addresses insurance fraud by combining voice and call intelligence with real-time AI automation to identify suspicious behavior from the First Notice of Loss (FNOL). It triggers fraud alerts, prioritizes risky claims, and facilitates quicker adjudication through data-driven decisions.
Insurers benefit by uncovering complex fraud patterns, integrating seamlessly with existing claims systems, utilizing transparent AI models for compliance, and reducing fraud losses while enhancing claim processing speed and accuracy.
When fraud is happening in real time, your defense should be too. Convin equips insurers with the tools to act faster, smarter, and at scale. Let’s look at what’s changing in the fraud scenario and how you can take control.
Stop fraud before it starts with real-time AI.
The Growing Cost and Complexity of Insurance Fraud
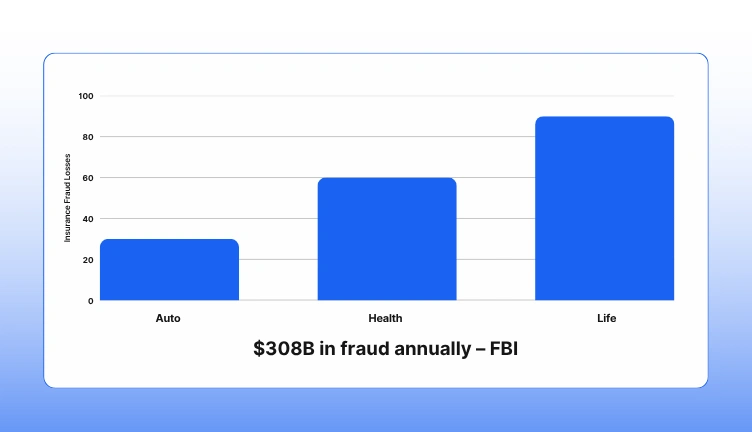
Insurance fraud is one of the most expensive and persistent threats insurers face today. The FBI estimates that fraud costs the industry over $308 billion every year, a burden that directly impacts profitability, premiums, and operational efficiency.
And it's only getting more complex.
Fraud is no longer limited to a few bad actors inflating claims. Today, insurers are dealing with:
- Organized fraud rings staging coordinated accidents and manipulating claims
- Synthetic identities are used to create fake policies and false claims
- Deepfake technology is producing altered voice recordings and fake documentation
- Medical billing schemes involving false treatments or upcoding
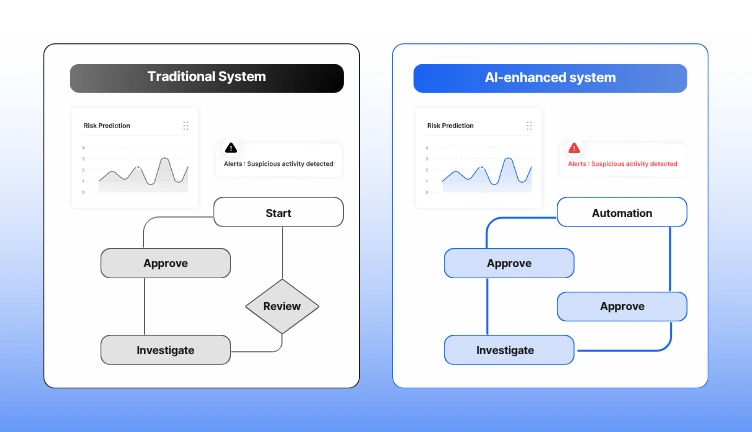
Manual audits, static red flags, and retrospective analysis are examples of traditional fraud detection techniques that are having difficulty keeping up. They rely on outdated logic and catch fraud only after the damage is done.
AI for insurance fraud detection can help with this.
With real-time fraud flagging, AI systems can scan incoming data as the claim is filed, identifying suspicious patterns instantly. For example, Convin’s AI listens to voice data during the First Notice of Loss (FNOL) and detects:
- Contradictory statements
- Hesitation patterns
- Anomalies in caller behavior
- Keywords and context cues associated with fraud
This real-time capability means insurers don’t need to wait for red flags to pile up. Instead, they can act immediately, saving time and reducing leakage.
The benefits of AI fraud prevention in insurance go beyond detection. It enables:
- Faster claim decisions for legitimate customers
- Reduced false positives, keeping investigators focused
- Scalable fraud monitoring across all business lines
Fraud is evolving. However, your fraud protection approach may remain one step ahead if you have the appropriate AI technologies in place. These tools are fast, accurate, and designed for real-time defense.
Fraud is rising: your detection needs to be faster, too.
What Real-Time AI and Automation Bring to the Table
Speed matters in fraud detection. The longer a suspicious claim sits unnoticed, the more likely it is to cost your business. Real-time AI solves this by identifying potential fraud the moment a claim is submitted or a conversation begins.
With insurance fraud detection AI, insurers can instantly analyze structured data and unstructured inputs like voice, text, and claim descriptions. Instead of relying on static rules, AI models learn from historical patterns, detect anomalies, and flag unusual behavior as it happens.
This shift from manual detection to automated risk scoring reduces human error and shortens decision cycles. Teams no longer wait for fraud indicators to stack up. They act at the point of contact, improving both speed and accuracy.
Real-time fraud flagging works across channels. Convin, for example, detects intent and inconsistencies during calls at the First Notice of Loss. It can identify hesitation, scripted responses, and tone changes that signal risk long before a traditional system would raise a red flag.
Automation makes this intelligence actionable. Once a claim is flagged, the system can:
- Assign risk levels
- Trigger alerts for review
- Move low-risk claims forward
- Launch automated investigations
The result is a streamlined workflow that keeps your fraud team focused and your claim cycle lean.
With AI fraud prevention in insurance, companies report measurable outcomes. These include faster case closures, reduced fraud losses, fewer false positives, and better resource allocation.
AI and automation are not just tools. They are enablers of a faster, smarter, and more scalable fraud prevention model. And they are ready to be deployed today.
Act instantly, detect smarter, prevent losses.
Key Benefits of AI-Powered Fraud Detection for Insurers
The pressure on fraud teams is rising. As claim volumes grow and fraud schemes become more complex, insurers need a faster, more accurate way to respond. This is where insurance fraud detection AI delivers real business value.
1. Real-time fraud flagging at the first touchpoint
AI can evaluate claims instantly as they enter the system. Whether it’s a digital form or a voice call at the First Notice of Loss, AI tools like Convin scan for risk signals in real time. This immediate fraud flagging helps prevent payouts on suspicious claims before they are approved.
2. Improved detection accuracy with fewer false positives
Traditional rule-based systems often trigger unnecessary reviews. AI uses historical data, context, and behavioral patterns to assess intent more accurately. This reduces false positives and allows fraud investigators to focus on the claims that actually need attention.
3. Faster claims processing for genuine policyholders
When AI quickly rules out fraud, legitimate claims can move forward without delay. This leads to better customer satisfaction, faster settlement times, and lower administrative overhead.
4. Cost savings through automation and smarter workflows
AI-powered systems reduce manual workload by automating detection, triage, and investigation workflows. With intelligent routing and risk scoring, your team spends less time on low-value reviews and more time on high-risk fraud.
5. Scalable, always-on fraud prevention
Unlike human teams, AI fraud prevention in insurance works 24/7. It learns from every claim, adapts to new fraud trends, and scales with your business across different lines - auto, health, property, or life.
By integrating AI into your fraud prevention strategy, you gain speed, precision, and control. It’s not just about stopping fraud. It’s about transforming how your organization handles risk in real time.
Discover how AI cuts costs, flags fraud, and speeds up claims.
This blog is just the start.
Unlock the power of Convin’s AI with a live demo.

Automation in Action: Use Cases Across the Claims Lifecycle

Insurance fraud does not occur at a single point. From the first report to the final settlement, it can be introduced at any point during the claims procedure. To effectively counter it, insurers need insurance fraud detection AI and automation built into each phase of the lifecycle.
Here’s how AI transforms every touchpoint into a smarter, faster, and fraud-aware operation.
1. Early Detection at First Notice of Loss (FNOL)
The moment a claim is filed, AI begins analyzing data in real time. Convin’s voice intelligence platform listens to customer calls and uses advanced models to detect signals of deception, hesitation, unnatural pauses, tone shifts, and scripted language.
This real-time fraud flagging happens instantly, before any human involvement. The system assigns a risk score and decides whether the claim should proceed, be escalated, or require further questioning.
Benefits at FNOL:
- Early detection prevents downstream fraud losses
- Low-risk claims are cleared faster, improving customer satisfaction
- High-risk claims are flagged for deeper review from the outset
2. Automated Evidence Collection and Analysis
Once a claim is flagged, AI systems automatically gather all supporting data, past claims, call transcripts, policy details, third-party information, and public records. Instead of spending hours compiling documents manually, investigators receive a pre-organized fraud dossier.
AI models also surface anomalies that a human reviewer might overlook. These include repeated claim behaviors, identity mismatches, or inconsistencies across timelines.
Benefits during investigation:
- Investigators are better equipped with contextual evidence
- Cases progress faster, with greater accuracy
- Risk signals are identified from multiple data sources simultaneously
3. Prioritization and Routing of Claims
Not every flagged claim carries the same risk. Automation helps insurers sort through volumes of data and assign claims based on risk severity, type of fraud, or urgency.
For instance, a high-value auto injury claim with repeat filing patterns may be routed to a senior investigator, while a lower-risk claim might only require digital verification.
Benefits of prioritization:
- Investigators focus on cases that demand expertise
- Case resolution times drop due to smarter routing
- Resources are aligned with fraud impact, not guesswork
4. Intelligent Decision Support at Adjudication
By the final stage, AI fraud prevention in insurance delivers a comprehensive risk profile for each claim. This enables adjusters to make informed, data-backed decisions: accept, reject, or hold for manual review.
AI-generated insights can also be configured to support compliance requirements, generating clear audit trails that explain why a decision was made.
Benefits during adjudication:
- Claims are processed faster, reducing cycle time
- Fraud leakage drops due to enhanced scrutiny
- Decisions are explainable and defensible for regulatory audits
Automation, powered by AI, brings structure, speed, and intelligence to every phase of claims handling. It not only reduces fraud losses but also boosts operational efficiency, enhances accuracy, and improves the overall customer experience.
With insurance fraud detection AI embedded end-to-end, insurers are better positioned to scale securely and stay ahead of evolving fraud risks.
What to Look for in a Real-Time AI Fraud Detection Platform
Investing in an AI solution to fight insurance fraud is a critical decision. Not all platforms are equal. Some may offer high-level analytics but lack operational depth, while others may promise automation but fail to integrate with existing systems. To ensure real impact, insurers should evaluate platforms based on five key capabilities.
1. True Real-Time Fraud Flagging: Timing matters. Your platform should detect suspicious activity the moment a claim is filed or a conversation begins. Look for systems that process data live, whether it's a web claim form, call transcript, or internal report.
Real-time fraud flagging prevents delays in detection, allowing teams to act before approval or payment occurs. This can significantly reduce financial exposure.
2. Advanced Behavioral and Pattern Analysis: Effective insurance fraud detection AI goes beyond basic keyword or rule-based checks. It must analyze behavior, voice tone, intent, and historical patterns across multiple channels.
Platforms should leverage machine learning models trained on real fraud cases to recognize subtle, complex signals, such as inconsistencies in speech or repeated filing patterns across structured and unstructured data.
3. Seamless Integration with Claims Infrastructure: A fraud detection system is only valuable if it fits smoothly into your existing claims workflow. Avoid solutions that require extensive rework or data migration.
The right platform should plug into your current claims management systems, CRM, and telephony stack with minimal disruption. It should enhance workflows, not create new complexity.
4. Transparent, Explainable AI Models: Trust and compliance are non-negotiable. Your fraud detection AI should offer clear insights into why a claim was flagged. This is essential not only for internal review but also for meeting regulatory and audit standards.
Explainable AI helps teams defend decisions, avoid bias, and build confidence in the system’s outputs.
5. Scalability and Customization
Fraud evolves constantly. Your solution must adapt to new patterns and scale across lines of business: auto, health, life, and commercial.
Platforms built for AI fraud prevention in insurance should allow customization of models based on geography, product type, and claim complexity. They should also learn from your historical data to fine-tune detection over time.
Choosing the right platform focuses on proven capability and adaptability rather than just aesthetics. An effective real-time fraud flagging system enhances fraud detection and improves the claims process, emphasizing the need for depth, flexibility, and intelligence that can evolve with the business.
Put AI to work at every step of the claims process.
Why Leading Insurers Choose Convin for Fraud Detection
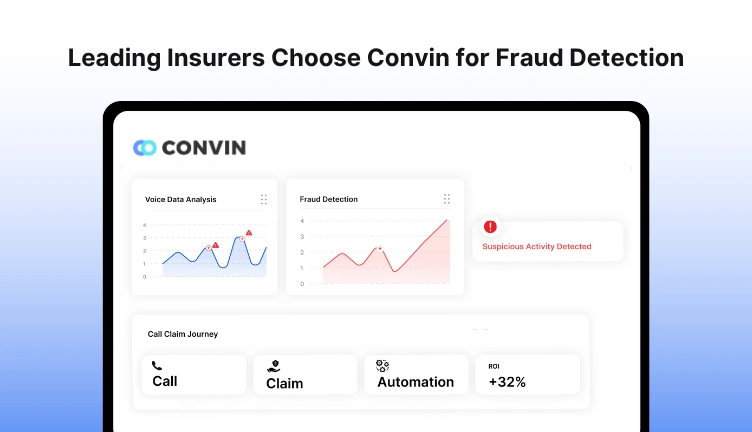
When fraud happens in real time, your detection strategy has to move faster than the threat. Leading insurers choose Convin because it enables them to detect, act on, and prevent fraud at the moment it surfaces and not after the damage is done.
Convin is not just another analytics tool. It’s a voice-first, automation-ready platform built specifically for the demands of modern fraud teams. By leveraging insurance fraud detection AI, Convin turns real-time customer interactions into the first and most accurate layer of fraud intelligence.
Here’s how Convin delivers where other solutions fall short:
- Voice AI that starts detecting fraud at FNOL
Convin listens to every claims call and analyzes it using behavioral intelligence, natural language processing, and sentiment detection. This allows the system to flag hesitation, scripted speech, tone changes, and inconsistencies during the First Notice of Loss - often before a claim is even formally submitted.
With real-time fraud flagging, your team receives actionable alerts based on voice cues, reducing the window of fraud opportunity and improving investigative speed.
- Automation from voice to investigation
Once a red flag is triggered, Convin’s automation engine kicks in. It creates a claim profile, assigns a risk score, and initiates the appropriate workflow. Whether the case requires escalation, additional verification, or documentation review, the platform routes it instantly.
This helps investigators focus on the right cases while ensuring no time is wasted on low-risk claims. It reduces manual work and speeds up fraud response cycles.
- Seamless integration with claims systems
Convin was designed to work with the systems you already use. It connects with CRMs, telephony platforms, and claims management software without disrupting existing workflows.
This makes onboarding fast and scalable - no need to overhaul legacy infrastructure. You gain modern AI capabilities without the friction of platform replacement.
- Transparent, explainable results
Every fraud decision made by Convin is backed by clear reasoning. Voice patterns, sentiment shifts, and claim inconsistencies are logged and visualized within the dashboard.
This supports internal teams in understanding why a claim was flagged and helps compliance teams meet audit and regulatory standards. Explainability is central to how Convin builds trust inside your fraud operation.
- Measurable ROI from day one
Insurers who adopt AI fraud prevention in insurance through Convin see measurable outcomes within the first few weeks. These include:
- Reduced false positives and shorter case resolution times
- Higher fraud detection rates and better loss prevention
- Improved customer experience through faster processing of genuine claims
- Enhanced team productivity without increasing headcount
Convin provides fraud detection that is quick, scalable, voice-aware, and built for real-time performance in order to meet the demands of the modern insurance industry. That’s why leading insurers trust Convin to help them stay ahead of increasingly complex fraud threats.
Close the Gaps in Your Fraud Defense
Fraudsters are getting faster, smarter, and more sophisticated. To stay ahead, your fraud strategy needs to match that speed with precision and automation.
Convin helps you do exactly that by combining real-time voice intelligence, advanced AI, and automation that fits right into your claims process.
Whether you're looking to reduce fraud leakage, improve investigator efficiency, or deliver faster resolutions to genuine customers, Convin gives you the tools to make it happen.
Book a demo with our experts and explore how Convin can help your team detect more fraud, act faster, and streamline investigations with confidence.
Frequently Asked Questions
1. How does insurance fraud detection AI handle deepfake or synthetic voice fraud?
AI models trained on large datasets can detect unnatural speech patterns, mismatched vocal tones, and inconsistent phrasing, making it harder for synthetic voice or deepfake scams to slip through undetected.
2. Can real-time fraud flagging work in multilingual or regional call centers?
Modern AI systems support multiple languages and dialects, enabling accurate fraud detection across diverse geographies and customer segments.
3. How secure is the data used in AI fraud prevention for insurance?
Top platforms like Convin ensure all data is encrypted, access-controlled, and compliant with regulatory frameworks such as GDPR, HIPAA, or ISO standards.
4. Does insurance fraud detection AI improve regulatory compliance?
By generating explainable outputs and audit trails, AI helps insurers meet compliance standards and document decision-making processes more effectively.
5. Is AI fraud prevention in insurance useful for post-claim audits too?
Absolutely. AI can be applied after claim settlement to identify overlooked fraud signals, refine models, and support special investigation units (SIUs) with historical pattern analysis.







.avif)