Lead-teams rarely pause to examine just how much time reactive claim queries consume, and what’s left unsold while answers are chased. In one recent survey, 79% of insurance customers want proactive updates on claim status.
That expectation is shifting claim-handling from back-office cost centre to strategic touchpoint, and sales teams are in the cross-hairs if status updates fall behind.
In the sections ahead, you will explore how claim status automation reorganises workflows from intake to payout, aligns CX and sales around the same timeline, and frees your reps to sell , not service.
You’ll see how technologies like real-time agent assist and conversation intelligence power this transformation, and how platforms like Convin help deliver measurable gains. You’ll walk away with actionable frameworks and metrics to turn status updates into selling time.
Use Convin to automate claim updates and keep teams aligned at every stage
The Hidden Cost of Reactive Claims Status Handling
When claim updates are managed reactively, every unresolved status becomes a call waiting to happen.
In fact, contact-centres often face rising volumes simply because customers don’t receive timely information, one industry study shows that 61 % of care-leaders report higher call volumes linked to poor status visibility and resource forecasting.
That surge isn’t just a nuisance: it eats into your sales-team’s time, disrupts CX reps, and creates a hidden cost centre under the guise of service.
By shifting the dynamic from answering to informing, you can begin reclaiming hours, reducing interruptions, and aligning sales & CX around the same rhythm.
1. Inbound spikes and how they steal selling time
Inbound call spikes happen when customers feel left in the dark about their claims. Without claim status automation, they turn to the contact centre for answers, creating traffic that overwhelms both CX and sales teams.
A new study shows claims-related calls account for up to 55% of all insurance service inquiries, making them the single largest driver of inbound volume.
This level of avoidable volume eats into selling hours fast. Sales teams lose momentum each time they’re pulled into claim-related escalations, and CX agents spend significant portions of their shift handling repeat inquiries that don’t move the claim forward.
The cumulative effect is fewer lead conversations, slower follow-ups, and reduced efficiency across the entire revenue engine.
Keeping customers proactively informed through claim status automation prevents these demand surges and gives sales teams the uninterrupted time they need to close business and engage meaningfully with prospects.
2. How poor status visibility undermines CX and sales alignment
When claim status is dispersed across disconnected systems, both CX rhythm and sales timing fracture. Customers expect transparency throughout the lifecycle, yet recent data shows only 51% of auto-insurance customers trust their insurer.
Sales teams feel this gap when they engage customers still processing uncertainty. Without real-time insight into claim status or proactive updates via automation, reps risk reaching out at the wrong time, pitching when trust is low, or missing opportunities altogether.
Meanwhile CX agents are working without the full picture, learning of delays only post escalation.
When sales and CX share unified visibility into the claim automation process, you align expectations internally, reduce escalations, and rebuild customer trust one interaction at a time.
Start aligning your teams with clear, real-time claim status visibility today.
Claim Status Automation: What It Is & How It Works
When status updates happen automatically, you shift from answering questions to avoiding them. That’s the essence of claim status automation, integrating rule-based workflows, real-time triggers and self-serve updates so customers don’t need to call.
For example, insurers using automation have cut processing time by as much as 60% and reduced manual error rates significantly.
This capability isn’t limited to back-office efficiency, it fundamentally alters the claim automation process, delivering faster status clarity, fewer inquiries and a smoother experience for both CX and sales teams.
1. From intake to payout: key stages in the claims automation process
The journey of a claim, from first notice through to payout, defines where inefficiencies lie and where automation creates the most value.
The process begins with intake: digital submission of policy and incident data, replacing paper forms and manual entries. Then comes triage and validation: the claim is automatically routed, reviewed, and checked for completeness.
Next is assessment and decisioning: damages or losses are evaluated often using AI or predefined rules. Finally, the payout or settlement stage occurs, where funds are released and status updates are communicated to the policyholder.
According to industry research, insurers implementing automated workflows across these stages reduce their manual intervention time and error rates significantly. For example, carriers using automation see streamlining of claims tasks that once took days trimmed down to a matter of hours.
This end-to-end view of the claim automation process is vital for CX and sales teams: each stage produces status updates, touchpoints and potential friction. When you automate these stages and integrate visibility, you reduce the hand-off errors, reduce delays, and keep the customer informed at every step.
Viewing claim automation through this intake-to-payout lens helps you identify where status updates matter most, and where proactive automation amplifies both service quality and selling capacity.
2. Core technologies and features that power status automation
Behind claim status automation, technologies like AI-based document extraction, rule engines, real-time event triggers and self-service portals are doing the heavy lifting.
For instance, more than 82% of insurers now deploy AI in their claims processes, and these systems handle roughly 31% of claim volumes in 2025, dramatically reducing cycle times.
Key capabilities include automated intake forms that pre-populate from policy data, decision-logic engines that route or approve simple claims, and portals/app notifications that update customers at each checkpoint, eliminating many status-calls.
When you layer these features into the status process, you enable CX teams to anticipate issues and sales teams to manage pipeline timing more accurately.
Automated triggers inform customers of progress, approvals or required actions before they call. Status dashboards give agents and reps a clear view of where each claim stands, avoiding surprises and enhancing coordination.
Power your claim updates with Convin and create real-time visibility for teams.
This blog is just the start.
Unlock the power of Convin’s AI with a live demo.

From Status Updates to Selling Time: The Sales & CX Advantage
When your teams stop chasing every “Where’s my claim?” call, they gain time to sell instead of being stuck in status updates.
Recent research shows that 44% of policyholders “research what it’s like to make a claim with a given insurer before buying”, meaning your claims handling impacts sales too.
With proactive status communications powered by automation, reps spend less time answering inbound spikes and more time moving the needle. Now let’s examine how exactly that shift creates value across sales and CX in measurable ways.
1. How proactive status updates deflect complaints and reduce call volumes
When customers receive timely, automated updates about their claim status, the number of basic status-inquiry calls drops significantly. Research by Accenture found that around 40% of inbound claims calls are simply status checks.
By deploying proactive messaging, sales and CX teams stop reacting to the same question over and over. Instead of reps being diverted into claim-status triage, they focus on meaningful engagements.
Automated updates via email, SMS or app push keep policyholders informed before they decide to call. The result: lower volumes of repetitive calls, reduced agent strain, and fewer complaints climbing into the escalation queue.
With fewer interruptions and better status visibility, your teams can maintain workflow steadier and more concentrated.
2. What sales leaders gain? More time, better focus, higher conversion
When status-related tasks shrink, sales leaders can drive tangible gains across performance metrics. With fewer agents pulled into complaint handling and fewer status queries clogging pipelines, sales reps reclaim hours to engage leads, renewals and cross-sells.
According to an overview by Innovation in Business, insurers adopting automation in claims processing report up to 30% cost reduction and increased capacity for higher-value work.
More time means sharper focus: reps tailor conversations rather than get sidetracked into servicing. Lead conversations become richer, conversion rates improve, and cross-sell opportunities increase.
Improved service and fewer complaints recycle into better trust and shorter deal cycles. A streamlined claim status flow is an enabler of sales productivity, not a drain.
Activate Convin’s status automation and convert more customers now.
How Convin Enables Claim Status Automation at Scale
Scaling claim status automation takes more than workflow rules. It requires visibility into every conversation, every repeated query, and every point where customers lose confidence. That’s the layer most insurers miss.
Convin closes that gap by turning real conversations into signals your teams can act on. With real-time guidance, interaction analysis, and customer-voice intelligence, Convin helps insurers automate status updates with accuracy while reducing the operational drag on sales and CX.
This creates a system where customers stay informed, agents stay confident, and sales teams stay focus
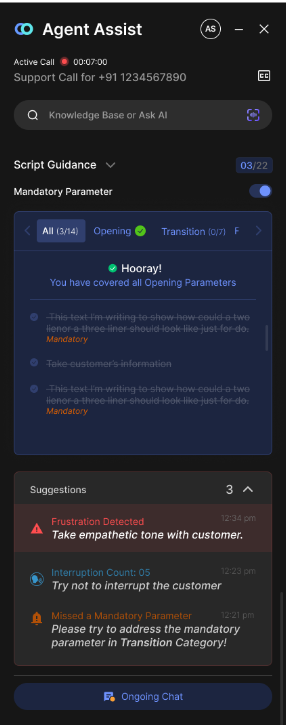
1. Key features: real-time agent assist, conversation intelligence, voice-of-customer, sales-calls analytics
Claim status automation only works at scale when frontline teams have clarity, context, and support during every interaction. Convin strengthens this foundation through capabilities that work together in real time.
Real-time Agent Assist guides agents with prompts, compliance reminders, and next-step cues during claim-related calls, reducing errors and shortening handling time.
Conversation Intelligence captures and analyzes every interaction, surfacing common friction points like repeated status-check questions or unclear claim steps. This builds a continuous feedback loop for CX and operations teams.
The Voice-of-Customer layer brings context that most insurers miss. It identifies sentiment shifts, detects emerging claim issues, and reveals patterns that impact customer trust. This is essential when research shows only 17% of insurers deliver a truly seamless omnichannel experience, leaving large visibility gaps in claim interactions.
Convin’s sales-calls analytics completes the picture by showing where sales teams lose time due to status inquiries, escalations, or miscommunication. With this insight, leaders can redesign workflows, eliminate repetitive effort, and ensure claim automation supports, not distracts, sales productivity.
Together, these capabilities create a connected, proactive system where claim status automation benefits every team, not just operations.
2. Case data and stats: efficiency gains, complaint deflection metrics, ROI
The impact of claim status automation becomes clear when you examine measurable outcomes across insurers. A global claims study found that carriers leveraging advanced automation tools improved processing accuracy by up to 30% and reduced cycle times across key claim categories.
These efficiency gains translate directly into fewer customer escalations, lower operational load, and stronger financial performance. Public research shows that automated claims environments can decrease cost per claim by 25–40%, primarily because fewer manual interventions and fewer status-related calls strain the system.
Convin’s analytics deepen this ROI by identifying where status inquiries originate, which journeys create repeat calls, and how agent behavior shapes complaint volume.
By combining automation with insights, insurers can deflect avoidable calls, reduce complaint recurrence, and recapture time across CX and sales teams, results that compound quarter after quarter.
Unlock higher ROI from every claim status workflow with Convin today.
Making Claim Status Automation Strategic: The Next Step
Claim status automation is no longer an isolated operational upgrade. It shapes how customers experience every part of the insurance journey and determines how much productive time CX and sales teams can recover.
When updates are proactive, status calls drop, complaint patterns shift, and the organisation gains predictable control over service demand.
For sales leaders, the impact is direct: fewer status interruptions, sharper lead engagement, steadier pipeline movement, and higher-quality customer conversations.
For CX leaders, it removes the constant pressure of repetitive call loads and provides the clarity needed to manage capacity. Together, these improvements create a more coordinated rhythm across teams and reduce the frictions that slow down growth.
Convin brings these advantages into one system, real-time agent support, conversation intelligence, customer-voice insights, and sales-call analytics working together to modernise the claim automation process.
With clearer visibility and automated status transparency, teams move faster, customers stay informed, and leaders gain a stronger handle on performance. If you're ready to build a proactive claim experience that fuels both service and sales momentum, the next step is here.
Book your Convin AI demo today!
FAQ
1:How does claim status automation reduce inbound call volume?
Claim status automation sends customers timely, proactive updates, removing the need to call for basic information. Since a large share of inbound traffic is status-related, automated notifications deflect these calls before they reach CX or sales teams. This creates fewer interruptions and steadier workloads across the organisation.
2: Why should sales leaders care about claim status automation?
Sales teams lose selling time when they’re pulled into claim-related escalations. Claim status automation prevents these diversions by keeping customers informed and reducing complaint spikes. With fewer reactive tasks, sales reps focus on leads, renewals, and conversions, improving overall performance.
3: What technologies are required to automate claim status updates?
A complete setup includes automated workflows, real-time triggers, decision engines, and self-service channels that push updates across email, SMS, or apps. Platforms like Convin enhance this by adding conversation intelligence, agent guidance, and customer-voice analysis to strengthen accuracy and visibility.
4: How does Convin support claim status automation for CX and sales teams?
Convin brings all interaction data into one system, analyzing calls, identifying claim-status patterns, guiding agents in real time, and surfacing customer sentiment. This improves accuracy, reduces avoidable escalations, and helps both CX and sales teams stay aligned throughout the claim automation process.








.avif)